Everyone experiences time away from their social circles occasionally, but experiencing continual social isolation comes with its risks. Chronic social isolation is just as harmful as smoking, according to an advisory report from the surgeon general. And the risks of social isolation continue to grow worse.
“Loneliness is far more than just a bad feeling – it harms both individual and societal health,” U.S. Surgeon General Dr. Vivek Murthy said in his report. “The mortality impact of being socially disconnected is similar to that caused by smoking up to 15 cigarettes a day. And the harmful consequences of a society that lacks social connection can be felt in our schools, workplaces and civic organizations, where performance, productivity and engagement are diminished.”
Today, more than half of U.S. adults report feeling disconnected from others and experiencing loneliness in their daily lives. And despite the large prevalence, less than 20% of adults who often or always feel lonely actually view their loneliness as a major issue.
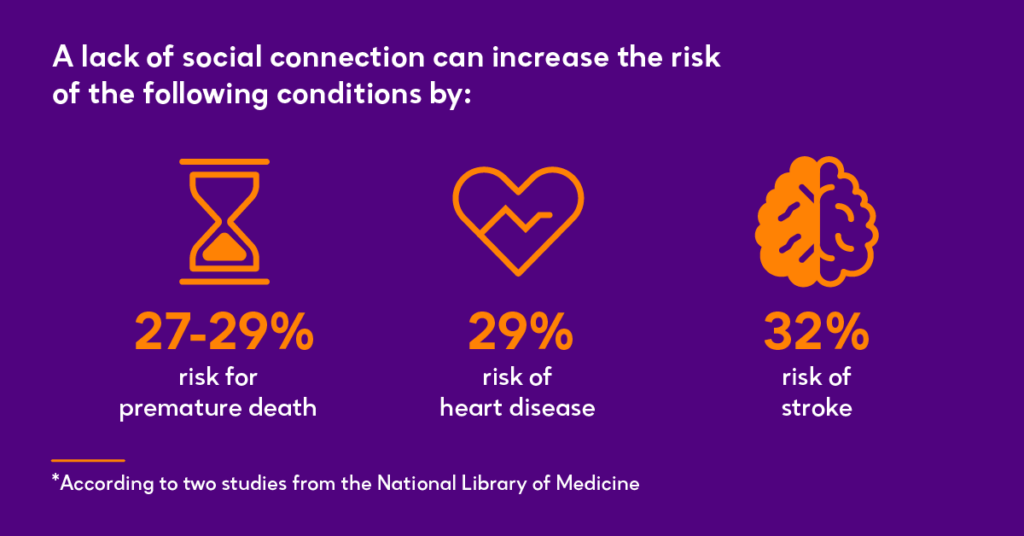
Lacking social connection poses a risk for premature death, an increased risk of disease, an increased risk of stroke and higher susceptibility to anxiety, depression and dementia.
Murthy’s report calls attention to the importance of social connection. He declares loneliness and social isolation a public health issue, especially after the prolonged social isolation society faced due to the COVID-19 pandemic.
What is social connection?
According to the report, social connection refers to “the interactions, relationships, roles and sense of connection individuals, communities or society may experience.”
Generally, social connection has three parts: the structure of one’s relationships with others, the function of how others can fill one’s needs and one’s quality of relationships.
Over the past few decades, the rates of social connection in the American population have declined. According to the report, Americans are increasingly less trusting of others. They spend more time alone and less time in their community.
What is social isolation?
The definition of social isolation is a lack of social relationships, roles, groups and overall infrequent interaction with others. Social connection is the fix to social isolation. But social connection is a two-way street, relying on at least two parties to put in effort toward increasing connection.
For older adults, this can become an issue when they don’t realize their social isolation may be contributing to their poor physical or mental health.
The risks of social isolation in older adults
Adults over 65, or retirees, have increased amounts of time for leisure – but also for social isolation.
Older adults are in fact at the highest risk of social isolation, considering the majority of them either live alone or deal with poor health status. In addition to poor health, they often face hearing difficulties, decreased amounts of driving or challenges with technology –three things that can make connecting with others more difficult.

Additionally, chronic loneliness and social isolation actually increase the risk of developing dementia in older adults by 50%, according to a study cited in the report.
Not only does social isolation affect the patient, it affects the health care system as well. The increased time spent alone in the 65+ age group results in $6.7 billion in excess Medicare spending annually, studies have found. This is due to an increased use of hospitals and assisted living facilities, as older adults may not have a wide network of people to take care of them.
“We want older adults who feel this way to know that Enhabit can help,” Executive Vice President of Clinical Excellence & Strategy Bud Langham said. “Our team takes pride in developing deep, personal relationships with patients so that we can really focus on treating the whole person. During the transitional period where patients are confined and recovering at home, we make sure to carefully monitor signs of social isolation, prioritize education and promote self-management using evidence-based tools and best practice interventions to help older adults take control of their health care journey.”
How can health care professionals address the risks of social isolation?
Murthy sees the risks of social isolation as a threat to each American’s health. The advisory report suggests ways that health care professionals can help combat social isolation:
- Acknowledge that social isolation is an issue and a risk to patient health.
- Remain up-to-date on current knowledge of social isolation and how it negatively affects patient’s health.
- Provide education to patients regarding the risks of social isolation and how to take action to avoid negative impacts to their health.
- Integrate social connection into the care you provide by evaluating where each patient’s risk level is and using psychosocial support to meet them where they are.
- Get connected to local community organizations that can provide resources to at-risk patients.
How home health can help address the risks of social isolation
It is crucial for health care professionals to know how chronic health issues impact patients’ psychological and emotional health. Whenever a patient is unable to leave their home due to a chronic condition or injury, that raises their risk level for social isolation.
If the patient is eligible for home health services, home health clinicians will educate them on their condition and provide practical management strategies to help patients improve their quality of life.
And as a part of home health clinicians’ initial assessments of patients, Medicare requires clinicians to ask about the patient’s self-reported levels of loneliness and isolation and pass their answers along to the patient’s physicians. That way, the physician can adjust their plan of care specificially to help reduce feelings or risks of social isolation.
Home health clinicians can also work across disciplines to connect patients to resources that can help them meet their specific health care goals. This includes how to lower their risk of social isolation.
When John began receiving home health care from Enhabit, he was living with high-risk depression and elevated feelings of loneliness. See how the Enhabit team helped increase his quality of life.
“At Enhabit, we take a person-centered approach to ensure each patient achieves their specific health care goals,” Langham said. “Every clinician plays an integral part in safeguarding the wellbeing of all persons entrusted in our care. When one person on the team notices a patient is struggling, they are encouraged to bring it to attention immediately. That way, we can equip the patient with the emotional or mental health resources they need in addition to their skilled medical care.”
For over 20 years, Enhabit Home Health & Hospice has provided high-quality, compassionate care to every patient wherever they call home. As one of the nation’s largest Medicare-certified home health and hospice providers, learn how Enhabit is expanding what’s possible for patient care in the home.
Social Share
At Enhabit our patients are our number one priority. From providing the latest medical practices to building deep personal connections, we’re focused on upholding every patient’s dignity, humanity and sense of control on their health care journey.
Home health
Our home health services give patients access to the care they deserve in the comfort of their own homes. From disease and injury management to recovery from surgery, our clinicians help patients confidently achieve their healthcare goals.
Hospice care
Our hospice care services place importance on the comfort of every patient living with a terminal illness. Our caring professionals are dedicated to providing not just physical care, but spiritual and emotional support to every patient and their loved ones.





